Rheumatoid Arthritis vs. Osteoarthritis: Symptoms, Causes, and What to Do Next
Do stiff joints and daily pain hold you back from performing at your best? Whether you live an active lifestyle or your career revolves around pushing your body to the limit, joint problems aren’t just an annoyance – they can significantly impact quality of life.
The first step to recovery is pinpointing the cause. Arthritis is one of the most common reasons for joint pain [1]. However, many people mistakenly think of arthritis as one umbrella condition. In reality, the two main types of arthritis – osteoarthritis and rheumatoid arthritis – are quite different, with varying recovery strategies.
When it comes to both rheumatoid and osteoarthritis, conventional medicine tends to focus on addressing physical decline. Pain medicines are often used to manage symptoms, but their relief is short-lived. Regenerative medicine, on the other hand, centers around long-term restoration. At RMI Health, we use cutting-edge stem cell therapy to alleviate pain and bring back mobility. That’s why RMI is one of the best stem cell clinics in the world.
What is the Difference Between Osteoarthritis and Rheumatoid Arthritis?
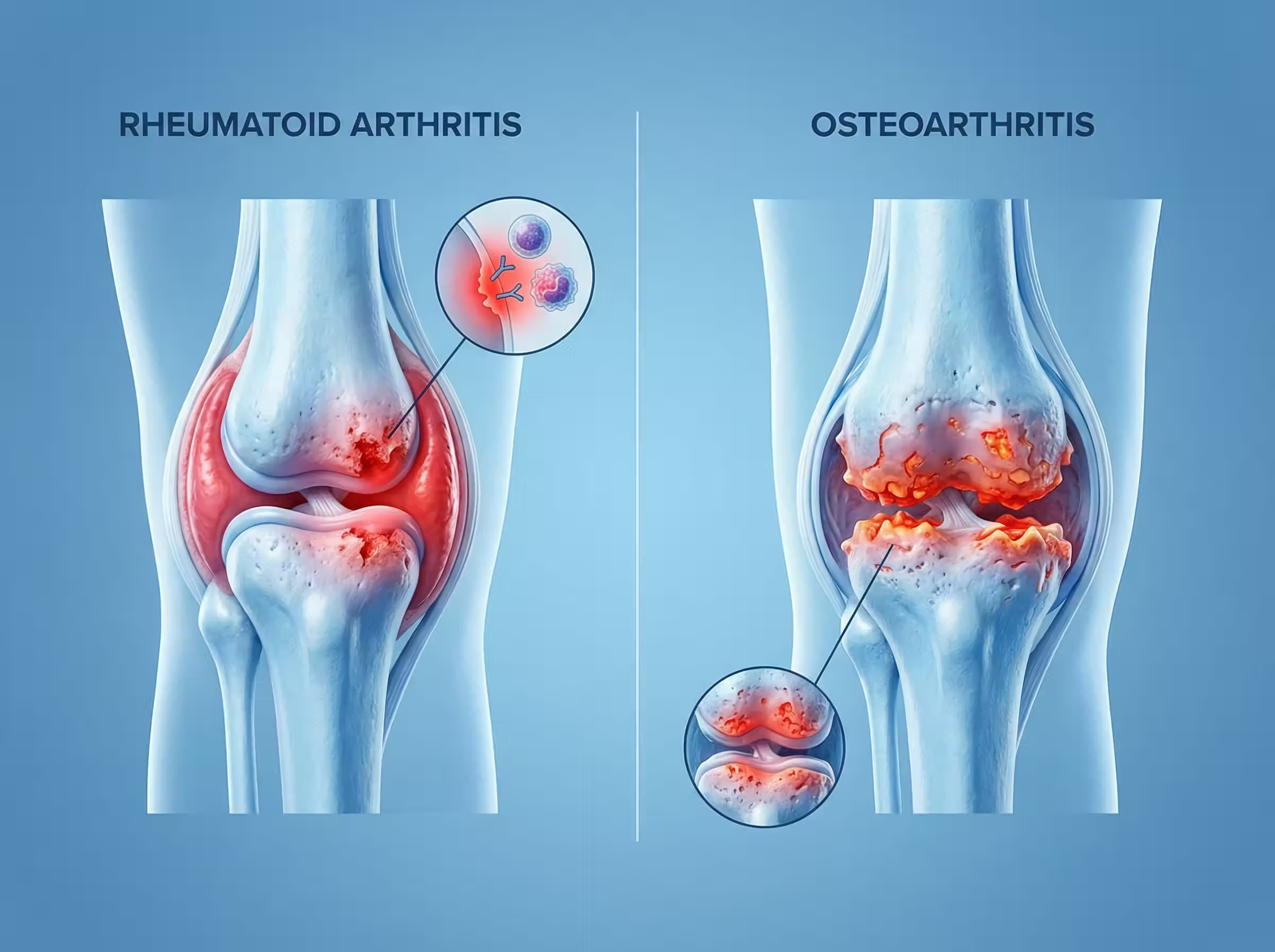
Osteoarthritis and rheumatoid arthritis are both joint conditions. While there are overlaps between the signs and symptoms of each form, there are many differences that set them apart – the most significant being the cause.
Rheumatoid Arthritis vs Osteoarthritis
(typically in the hands)
Rheumatoid Arthritis (RA)
What is Rheumatoid Arthritis?
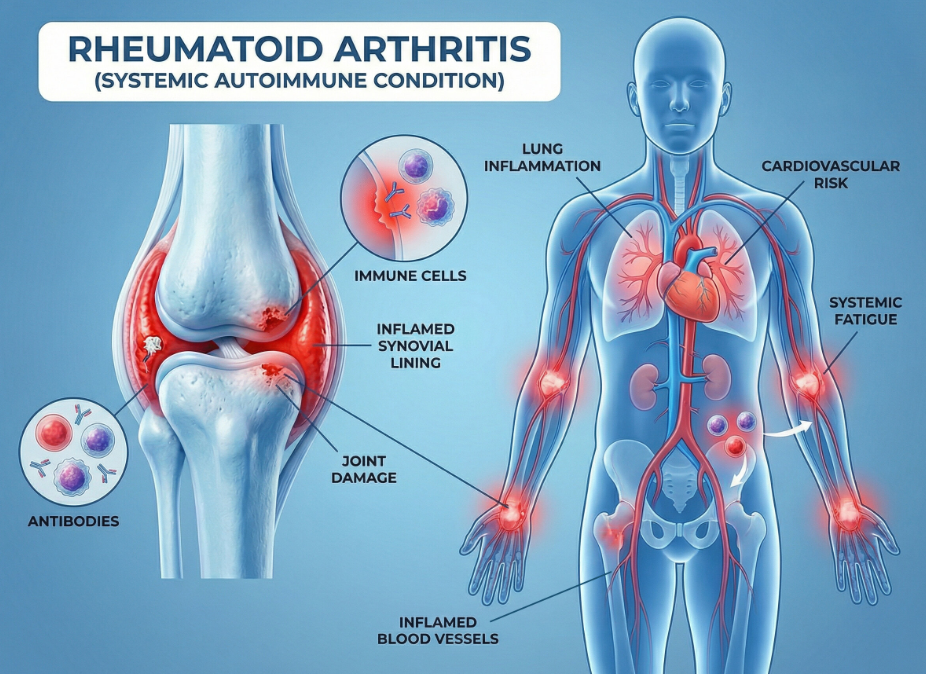
Rheumatoid arthritis is a chronic autoimmune disease that causes inflammation and progressive joint damage. It occurs when the immune system mistakenly attacks the tissues lining the joints, known as the synovium. Over time, this causes some joints to become inflamed, painful, and swollen. Everyday activities such as writing, walking, and holding objects can become very difficult.
Joint pain is the most common symptom of rheumatoid arthritis; however, the condition is systemic, meaning it affects the entire body. If left untreated, rheumatoid arthritis can deform joints and seriously damage other parts of the body, including the skin, heart, lungs, and nervous system.
What Causes Rheumatoid Arthritis?
Researchers are still working to determine the root cause of rheumatoid arthritis. Current evidence points to a complex mix of environmental and genetic factors [4]. For example, specific genes are linked to a higher risk of developing rheumatoid arthritis. In people with those genes, behaviors such as smoking and obesity may further compound their risk. Exposure to certain viruses or bacteria may also trigger the disease in people who are genetically predisposed.
The severity of rheumatoid arthritis also appears to be linked to external factors such as high stress levels. A 2025 study by the University of California, San Francisco, found a link between higher stress and worse pain in rheumatoid arthritis patients [5].
What are the Key Symptoms of Rheumatoid Arthritis?
There are two main categories of rheumatoid arthritis symptoms: joint and systemic.
Joint symptoms:
- Pain
- Swelling
- Redness
- Warmth
- Tenderness
- Morning stiffness – usually lasting over 30 minutes before improving.
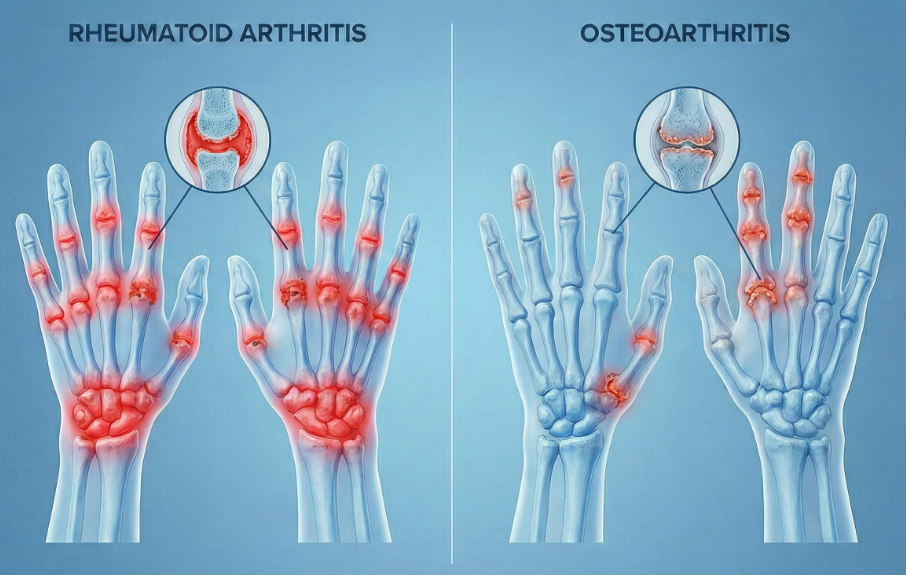
The joint symptoms associated with rheumatoid arthritis are usually symmetrical; this means they affect the right and left sides of the body at the same time – for example, both wrists or both knees. At late stages, untreated rheumatoid arthritis can cause joint deformity and destruction.
Systemic symptoms:
- Significant fatigue
- Low-grade fevers
- Loss of appetite.
Rheumatoid arthritis may also have serious effects on other parts of the body, such as the skin, heart, lungs, and nervous system if left untreated.
It’s common for rheumatoid arthritis symptoms to change over time. Some people may have flare-ups, where their joints are particularly painful, before going long periods without any symptoms.
What Joints Are Affected by Rheumatoid Arthritis?
In most cases, rheumatoid arthritis starts in smaller joints, such as the knuckles (MCP or metacarpophalangeal joints) or middle joints of the fingers (proximal interphalangeal joints).
It often also affects the:
- Wrists
- Hands
- Balls of the feet
- Ankles
- Knees
- Shoulders
- Elbows.
How is Rheumatoid Arthritis Diagnosed?
Doctors typically look at a range of factors before concluding someone has rheumatoid arthritis. Diagnosis is made by the clinical picture, so they will consider symptoms and medical history, along with tests such as:
- X-rays
- Blood tests to find markers of rheumatoid arthritis
- Imaging, such as ultrasound or MRI, to look for inflammation or damage.
Osteoarthritis (OA)
What is Osteoarthritis?
Osteoarthritis is a joint condition that worsens over time. The disease breaks down the cartilage that cushions the ends of bones in a joint over time. This loss of cartilage causes the bones to rub against each other, leading to friction, pain, and reduced mobility. Osteoarthritis impacts the entire joint, including the surrounding tissue, bone ligaments, and tendons.
Typically, osteoarthritis is a mechanical issue from lifetime use – that’s why it often occurs in people over 55 years old.
What Causes Osteoarthritis?
Wear and tear is a major risk factor for osteoarthritis. A history of injuries to the joint, such as fractures and strains, is thought to speed up the condition’s onset.
Other factors that increase the risk of osteoarthritis include:
- Intensive athletic activity
- Heavy lifting and load-bearing
- Obesity
- Family history of the condition.
Aging is among the biggest contributing factors – and one that can’t be avoided. The body’s cartilage naturally loses water content and resilience, which makes it more likely to break down over time.
What are the Key Symptoms of Osteoarthritis?
The key symptoms of osteoarthritis are:
- Pain that tends to worsen during or after activity, and improves with rest
- Reduced range of motion – for example, trouble fully bending or extending a joint
- Grating or clicking sounds and/or sensations when moving affected joint(s)
- Tenderness when touching the affected joint(s).
Symptoms of osteoarthritis are not usually symmetrical. For example, someone may have joint pain in the fingers of their right hand, but not their left.
What Joints Are Affected by Osteoarthritis (OA)?
Osteoarthritis is most common in the:
- Knees
- Hips
- Spine – especially the lower back
- Neck
- Joints in the hands and feet, such as the thumb and big toe.
How is Osteoarthritis diagnosed?
In many cases, doctors diagnose osteoarthritis based on symptoms and medical history. If they are unable to determine what type of arthritis you have, they may refer you for tests such as X-rays or blood tests.
Which Is Worse: Osteoarthritis or Rheumatoid Arthritis?
Clinically speaking, rheumatoid arthritis is thought to be the worse condition. This is mainly due to its impact on the entire body and potential to damage vital organs – especially if left untreated. However, osteoarthritis can be just as debilitating and have major effects on a person’s life. It can impede daily mobility, making it hard to do simple tasks like walk up a flight of stairs.
Why can Conventional Treatments Fall Short for RA and OA?
Conventional approaches to treating rheumatoid and osteoarthritis tend to have two main goals: controlling symptoms and slowing progression.
Rheumatoid arthritis
Disease-modifying therapies or ‘DMARDs’ (disease-modifying antirheumatic drugs) are the most common treatment for rheumatoid arthritis. They aim to protect the joints and control inflammation driven by the condition.
Many work by regulating parts of the immune system and reducing immune response [6].
Their impacts on the immune system may increase the risk of infection.
They may also cause side effects such as stomach pain and liver problems [6].
In cases of severe rheumatoid arthritis and complete joint destruction, doctors may recommend surgery for joint replacement.
Osteoarthritis
Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly used to control osteoarthritis symptoms.
Injections into the joints provide temporary pain relief and help mobility.
Corticosteroid and hyaluronic acid injections are the most common.
Long-term use of steroid injections may actually accelerate joint degeneration [7].
Physical therapy is often recommended to reduce pain and support mobility.
Managing symptoms is important, but it can feel more like maintenance than long-term recovery and repair – especially for those who want to stay at peak physical fitness. That’s why many high performers seek emerging, evidence-based treatments that acutely target joint biology.
Treating Arthritis with Stem Cell Therapy at RMI
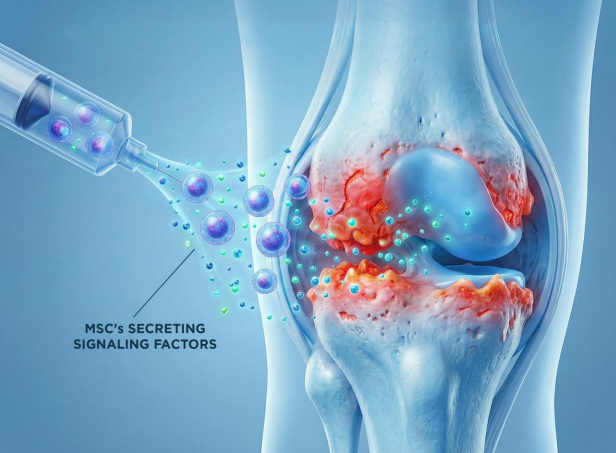
Stem cell therapy for arthritis centers around reducing inflammation and supporting tissue regeneration – not short-term pain relief.
At RMI Health, all of our regenerative treatments use stem cells called umbilical cord mesenchymal stem cells (UC-MSCs). These young and potent cells are derived from the donated umbilical cords of consenting patients who have given birth via C-section. There is no bone marrow or fat harvesting involved.
We use MSCs to treat arthritis. They work to ease inflammation and support joint function by secreting anti-inflammatory and regenerative factors; these factors act as messengers to immune cells [8]. There is a vast array of evidence supporting the safe use of MSCs for several human conditions, including arthritis [9]. Before use, our expert microbiologists rigorously test all MSCs for infectious diseases and ensure they are suitable for therapeutic use.
Our treatments for arthritis are non-surgical and generally have a fast recovery time, with some tenderness possible for a few days after.
How RMI Treats Rheumatoid Arthritis
We use intravenous (IV) stem cell therapy to treat rheumatoid arthritis. This circulates the MSC stem cells through the body via the bloodstream, helping to modulate the immune system and reduce overall inflammation.
How RMI Treats Osteoarthritis
Our physicians take a whole-joint approach to treating osteoarthritis. They perform clinical assessments and ultrasound to map areas of damage, before administering targeted joint injections using real-time ultrasound. Injecting stem cells directly into the damaged joints aims to reduce local inflammation and stimulate the body to repair the cartilage and other tissue.
Why Executives and Athletes Choose RMI in Costa Rica for RA and OA
Stem cell therapy in the US is an emerging field, but its scope is still limited. Current regulations restrict many treatments to the patient’s own autologous MSC stem cells; these may carry genetic defects and be less effective than MSCs from young and healthy donors [10]. Many executives and athletes instead head to Costa Rica for arthritis treatment with RMI Health.
Unlike the US, Costa Rica allows licensed clinics to use donated umbilical cord MSCs, which are robust, fast-replicating, and rarely rejected by the body. All clinics must adhere to strict quality and safety standards. It’s not a loophole treatment destination – it’s a regulated industry with oversight from the country’s Ministry of Health.
The Costa Rica RMI Health team is US-trained, with leading expertise in the field of stem cell regenerative medicine. Every patient is supported by our personalized concierge service throughout their recovery journey.
Ultimately, treatment in Costa Rica isn’t just about fixing knee pain; it’s about investing in health longevity.
Stop Managing Pain & Start Repairing It
Stop masking your symptoms with short-term treatments. Speak with our medical team to determine if stem cell therapy is the right strategy for your recovery.
CTA Button: [Request Your Medical Consultation]
FAQ
1. Can an MRI tell the difference between osteoarthritis and rheumatoid arthritis?
An MRI can help trained physicians determine whether a person has osteoarthritis or rheumatoid arthritis. While bones, cartilage, and soft tissue are affected by conditions, each has different characteristics. Trained physicians will often use an MRI alongside other clinical information, such as medical history and blood tests, to form an opinion.
2. Can osteoarthritis turn into rheumatoid arthritis?
Osteoarthritis cannot turn into rheumatoid arthritis, as they are separate diseases caused by different parts of the body. However, it’s possible to have osteoarthritis and rheumatoid arthritis at the same time.
3. What is the gold standard test for rheumatoid arthritis?
There is no gold-standard test for rheumatoid arthritis. Experienced doctors will typically consider medical history and risk factors for the disease alongside tests and imaging to reach a clear diagnosis.
4. What are usually the first signs of rheumatoid arthritis?
The earliest signs of rheumatoid arthritis are often morning hand stiffness, redness, and swelling of commonly affected joints such as wrists. People may also have systemic symptoms such as fatigue and fever. Sometimes, the first sign of rheumatoid arthritis is abnormalities on blood tests.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5732469/ (arthritis is one of the most common causes of joint pain)
- https://www.who.int/news-room/fact-sheets/detail/rheumatoid-arthritis (RA most common in 55+)
- https://www.aihw.gov.au/reports/chronic-musculoskeletal-conditions/osteoarthritis (Osteo most common in older)
- https://www.sciencedirect.com/science/article/pii/S2405580825002353 (genetic and environmental factors cause RA)
- https://pubmed.ncbi.nlm.nih.gov/40181767/ (greater stress = worse symptoms, UCSF study)
- https://www.ncbi.nlm.nih.gov/books/NBK507863/ (how to DMARDs work)
- https://pubmed.ncbi.nlm.nih.gov/38117096/ (corticosteroids may accelerate condition)
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6901025/ (MSC into bone and cartilage)
- https://www.sciencedirect.com/science/article/abs/pii/S0049017224001380 (safe use of MSCs for arthritis)
- https://www.sciencedirect.com/science/article/abs/pii/S1465324913004891 (MSCs are better from younger donors)



.svg)

.svg)